An Organizational Scholar Explains How to Learn from COVID-19
As of today, the United States has the highest number of COVID-19 cases and deaths in the world. With this level of human life destroyed, our society looks for not only solutions but lessons for the future. However, learning from a pandemic can be incredibly hard. Organizations rarely encounter them.1 How do we assign the credit and blame from this infrequent outcome to the myriad players, institutions, governments, and their actions? My research in organizational learning can help us outline how decision makers might learn when outcome-feedback is rare and infrequent.2
The last pandemic that reminds us of this level of destruction is the Spanish Flu, more than 100 years ago. Caused by H1N1 influenza A virus, it infected 500 million people (a third of world population) and resulted in a death toll as high at 100 million. Some Western states in the U.S. mandated citizens to wear masks and to socially distance while closing schools and public places. In the 102 years that have elapsed, there had been no pandemic that required similar measures or inflicted similar loss until COVID-19. Few living people had personally experienced the Spanish Flu, and even fewer had vivid memory of the draconian measures put in to combat its spread.
An even more extreme challenge is the 2004 Indian Ocean earthquake and tsunami, which created a series of massive tsunami waves as high as 30 feet and killed an estimated 230,000 people in 14 countries. Many governments were blamed for their lack of preparations. Yet, the last major tsunami in Indian Ocean occurred more than 700 years ago. No living beings personally experienced tsunamis to be so deadly. How can organizations, institutions, and societies prepare for, and learn from, something that occurs rarely, once in every 700 years?
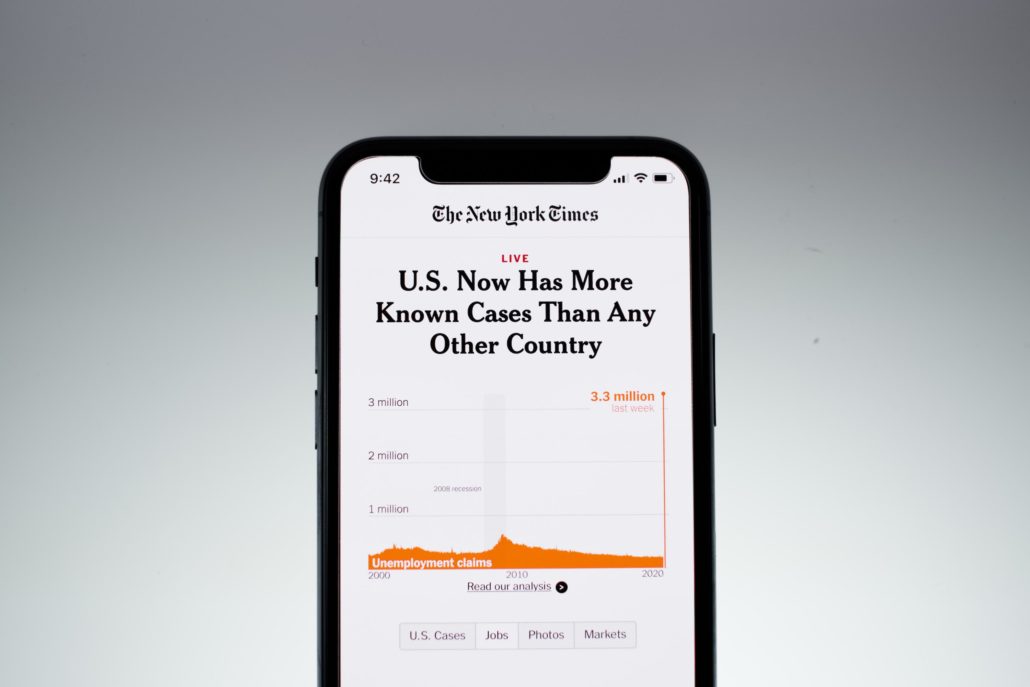
The worse a country did in SARS, the better it is doing so far in total deaths due to COVID-19.
First, decision makers need to attend to near histories—events that almost happened, such as successes improbably achieved or failures narrowly averted.3 In other words, when history is not generous with experience, organizations need to convert infrequent events into meaningful interpretations of history.
While memories of Spanish Flu may be distant, we have been given ample warning on hindsight. Sixteen years ago, the SARS Epidemic was caused by a then novel strain of coronavirus. It infected more than 8,000 people from 29 countries and caused more than 700 deaths worldwide. As compared to COVID-19, SARS is more deadly (fatality about 11 percent) and is similarly transmitted via respiratory droplets. Yet, the W.H.O. (the World Health Organization) declared SARS contained in July 2003, eight months since the outbreak started, without any vaccine, curative treatment, or even point-of-care diagnostic test.
In the years since the SARS outbreak, we have had time to reflect on the critical roles played by standard epidemiological interventions such as isolation, contact tracing, travel restrictions, as well as the strong leadership provided by the W.H.O. For instance, Hong Kong built a contact-tracing system from one initially used for crime investigations. Countries with major outbreaks installed temperature checks at airports to screen passengers. After the W.H.O. advised travel restrictions to affected countries, those areas saw travel decline by as much as 80 percent. SARS was, as a result, effectively contained within the Western Pacific region, where the virus was first discovered. Of the six countries and regions with more than five people dead of the virus, Canada was the only exception. The rest were Mainland China (349 dead), Hong Kong (299), Taiwan (73), Singapore (33) and Vietnam (five). In the vast majority of countries, SARS infections and deaths were both in the single digits. Based on the comparative loss of human lives alone, SARS is a spectacular victory as compared to the ongoing fight with COVID-19.
If SARS had been a dry run, then countries that suffered the most then have learned valuable lessons in the current crisis. Many physical capabilities remain—infrared temperature scanners, contact-tracing teams of experts, national systems of warning, et cetera. More importantly, the memory of SARS is still vivid. SARS had stimulated unprecedented media attention and heightened the perception of risks associated with a novel, and highly infectious, disease. Both private citizens and public servants learned a painful lesson: Political commitment and the successful management of public health are indispensable when there is no vaccine or drugs.
Subscribe to the Ethical Systems newsletter
As you can see in the figure below, there is a negative correlation between the rankings in total deaths due to SARS and the rankings in total deaths due to COVID-19 (at -0.15). In other words, the worse a country did in SARS, the better it is doing so far in total deaths due to COVID-19. Take, for instance, Hong Kong (ranked second) and Taiwan (ranked third) for SARS fatalities. Both countries have done well handling COVID-19—in terms of deaths, they are ranked at 113th and 146th, respectively. In contrast, most European countries were spared in SARS, yet have experienced record high number of COVID-19 deaths—Spain (fourth), the United Kingdom (fifth), Italy (seventh), Germany (ninth), France (12th).
For the U.S., SARS was a near miss from which we did not learn. Only 27 people became infected, none had died from SARS. The U.S. did not have a chance to build up necessary physical defense (like airport temperature checks), let alone develop community awareness and political will. From political leadership and public institutions to private individuals, the risk of COVID-19 was vastly underestimated from the get go. While ordinary citizens quickly put on masks in the Western Pacific countries as they did in SARS, masks became a culture-war weapon here. It did not help that the C.D.C.’s explicit guidance as of mid-March was that masks were only necessary for medical personnel when they treat patients with respiratory symptoms or fever. Only in the beginning of June did they update it based on a new study showing that N95s are superior to surgical or cloth masks.
Such underestimation of risk is also evident in the C.D.C.’s testing fiasco. For policy makers and the general public to realize the urgency of the matter, they need to have a working diagnostic test as soon as possible in order to know how many people are infected. The first diagnostic test for COVID-19 was developed by German scientist Olfert Landt on January 10th and vetted and published by WHO on January 17th. Yet the C.D.C. opted to create its own test from scratch. Delays and defects ensued and it was not until late February that a working test was sent out. During these crucial six weeks, infected individuals unknowingly passed through airports, hospitals, and communities, and the seeds of infections were sown.
If our own experience with an infectious disease with pandemic potential was limited, where else could we have looked for guidance? A second way for decision makers is to learn vicariously from others’ experience. We could have learned from other cities and countries who had the misfortune of being hit first and exploited the time these countries “bought” us. Here the challenge is also immense—how similar are we to other countries such as China and Italy, or to other cities such as Paris or Seattle? If we learn cautiously because we believe we are exceptional, little of others’ experience would have been directly relevant.4 With vicarious experience discounted, we are likely to react too slowly. However, if we think we are very similar to others, we would learn aggressively, but risk making mistakes that arise from overgeneralization of others’ experience. Thus, there is a speed-accuracy tradeoff; and our ability to extract valuable lessons from experience is anything but guaranteed.
Decision makers need to break free from theory and refocus on data.
New York City has the most COVID-19 fatalities, more than 22,000. The former head of C.D.C., Thomas R. Frieden, argued that had New York City adopted social-distancing measures a week or two earlier, the death toll there could have been 50 percent to 80 percent lower. Indeed, Seattle closed its schools five days earlier than New York City, and the rate of death is much lower. Was New York City so unique that lessons from other cities were deemed irrelevant? Many blamed close proximity in the city as its unique feature. Yet other world cities with similar populations have fared much better. Hong Kong, with a population of 7.45 million, has recorded only seven deaths, whereas New York City, with a population of 8.33 million, has recorded 22,103 deaths. We have failed to learn from other cities (Wuhan, Hong Kong, Paris, Seattle, San Francisco, and others) because somehow we believe New York City is exceptional.
Third, decision makers need to watch out for blind spots and competency traps that result from their own very success. Countries, cities, and organizations that survive over time typically do a few things very well and these competences may cause them to overlook systemic weaknesses. Part of the C.D.C.’s start-up troubles was that the group in charge of the COVID-19 response initially—the Division of Viral Diseases—was smaller and had far less staff focused on contagious respiratory diseases than the C.D.C.’s Influenza Division. While the U.S. had next to zero experience with coronaviruses, it had been a veteran of flu viruses of all kinds (swine, avian, among others). As such, the C.D.C. has developed far superior capability in the detection, management, and communication of the various flu viruses. Because of such superior capability and leadership in one area, the C.D.C. may have developed blind spots and underinvested in critical resources necessary for other less common yet more deadly viruses.
Lastly, decision makers need to break free from theory and refocus on data. When faced with a novel challenge (like 9/11 and COVID-19), existing theories about how the world operates can be irrelevant at best and misleading at worst. There needs to be rebalancing of the relative weights attached to theory derived from the past, versus the data gathered from the present. This is where the rigor and cautiousness of science may hinder the speed with which we evaluate and learn from clinical data. Theory is backward looking as it is distilled from past experience. In a new normal, decision makers need to weight much more empirical data about current trends. For instance, the W.H.O. had hesitated to prescribe masks as no scientific theory existed yet—only after the outbreak of COVID-19 did scientists begin well-designed studies to test the effectiveness of various personal protection equipment (such as masks, face shields) against the novel virus. While science progresses at the slow rate that promotes rigor, empirical and clinical data quickly pointed to the need for PPEs not only for medical personnel but also for everyday people. Japan, a country that had not shut down cities, nonetheless has done comparatively well in the pandemic as citizens simply follow their own laymen’s beliefs about wearing masks. This implies that decision makers need to take action guided more by data rather than by theory. It also implies that decision-making rights should be assigned to the front line workers in order to process the local cues that emerge from their daily work.
Organizational leaders need to attend to near successes or failures. These events are easy for leaders to overlook, because they are not outright successes or failures. For instance, an organization may have narrowly averted an accident, or a disaster. Since leaders typically wouldn’t see that as a failure, it does not tend to attract their attention. Yet near successes and failures, and how organizations deal with them, hold important lessons. Thus, leaders need to broaden their focus to include the less salient and extreme events in their own organizational history. Recording, analyzing, and learning from these is just as important as learning vicariously from the near successes and failures similar firms experience. Someone else’s disastrous accident, and its aftermath, can provide ample real-time simulations. Organizations at the very least need to have mechanisms in place to monitor, track, and analyze other players in their space (competitors, buyers, suppliers et cetera).
In a nutshell, how do decision makers begin to learn from rare events such as a pandemic? Taking a few ideas from organizational learning may help—attend to near misses, learn vicariously, watch out for competency traps, and downplay theory.
Christina Fang is Associate Professor of Management and Organizations at NYU Stern School of Business, where her research focuses on challenges and mechanisms of learning.
This post was originally published in Managing Organizations in a Time of Crisis, a series of research briefs produced by the Department of Management & Organizations at NYU Stern School of Business.
References
1. Lampel, J., Shamsie, J., and Z. Shapira, 2009. Experiencing the Improbable: Rare Events and Organizational Learning. Organization Science, 20(5), pages 835-845.
2. Fang, C. 2012. Organizational Learning as Credit Assignment – A Model and Two Experiments. Organization Science. 23(6), 1717-1732.
3. March, J. G., Sproull, L. S., & M. Tamuz. 1991. Learning from samples of one or fewer. Organization Science, 2(1), 1–13.Starbuck, W. 2009. Cognitive Reactions to Rare Events: Perceptions, Uncertainty, and Learning. Organization Science, 20, 925-937.
4. Starbuck, W. 2009. Cognitive Reactions to Rare Events: Perceptions, Uncertainty, and Learning. Organization Science, 20, 925-937.